Anal Fistula Surgery at Winfield Hospital
An anal fistula is a small tunnel (tract) that forms between your bowel and the surface skin near your anus. It can develop for a range of reasons, most commonly after a perianal abscess, and isn’t caused by poor hygiene or any other form of personal negligence.
Anal fistulas rarely resolve on their own and require surgical treatment. However, outcomes are generally positive, particularly when the operation is performed by an experienced colorectal surgeon.
To help you better understand anal fistulas and what the treatment involves, here we explain what they are, how they form, and anal fistula symptoms to look out for. We’ll also look at what you can expect from anal fistula surgery and recovery with Ramsay Health Care.
What is an anal fistula?
An anal fistula is a small, abnormal tunnel (tract) that forms around your anus.
The tunnel typically connects an internal opening (often in an anal gland) to an external opening on the skin near your anus. You can think of an anal fistula as an unwanted opening around your anus that runs into your body, usually connecting to your bowels. Sometimes, fistulas can create more than one opening on the surface of your skin, but one is the most common.
Fistulas often develop after a perianal abscess. This happens when an anal gland becomes infected, and a pocket of pus (mostly dead white blood cells, fluid, and bacteria) forms around the gland. When the abscess drains away, the pocket it creates can remain and can develop into a tunnel, especially if the pus drains via an opening on the skin, creating an anal fistula.
Anal fistulas affect around 1 to 2 people in every 10,000 (0.01 to 0.02% of people). They’re more common in men than women, with men roughly twice as likely to develop them.
They rarely heal on their own and usually require anal fistula surgery to treat them. While they aren’t usually a risk to your health, they can be painful and cause a range of symptoms that can affect your quality of life.
Types of anal fistulas
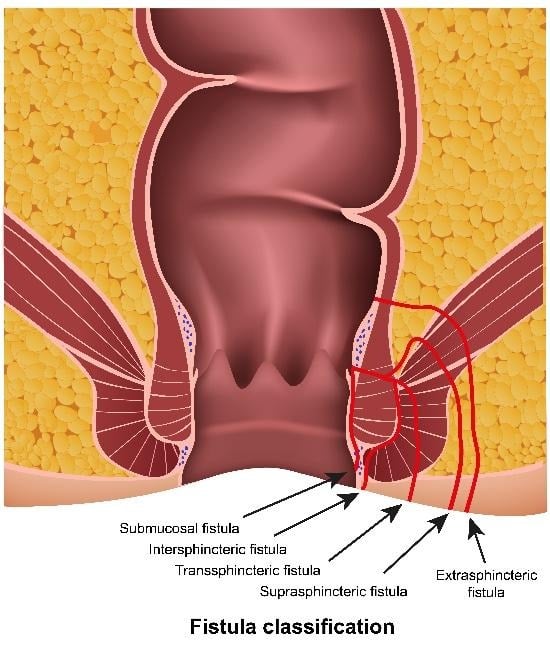
Anal fistulas are classified based on their location and their path into the body in relation to the anal sphincter muscles:
-
Intersphincteric anal fistulas - Form close to the anal opening and pass through the internal sphincter. These are the most common anal fistulas, accounting for approximately 70% of cases.
-
Transsphincteric anal fistulas – Pass through both the internal and external sphincter muscles. They account for approximately 25% of cases.
-
Suprasphincteric anal fistulas – Take a higher path over the sphincter muscles. They account for approximately 5% of cases.
-
Extrasphincteric anal fistulas - These are much rarer types of anal fistulas that take a complex path through the body and account for approximately 1% of cases.
Classifying what kind of anal fistula you have is important as it influences the surgical approach required and the potential risk to your continence (your ability to control your bowel movements).
Anal fistula symptoms
Anal fistula symptoms can vary, but they often significantly impact your quality of life.
The primary symptoms of anal fistulas include:
-
Visible opening(s) forming on the skin near the anus.
-
Discharge from the fistula opening, which may be pus, blood, or clear fluid, and can be constant or intermittent.
-
Discomfort and pain around your anus, which may worsen during bowel movements or when sitting for long periods.
-
Swelling and redness around the anus.
-
Irritation and itching of the skin around the anus.
-
Recurrent perianal abscesses (where an abscess drains and then reforms again).
Other associated symptoms of anal fistulas can also include:
-
Fever and fatigue, if an infection is present.
-
An unpleasant odour from the discharge, which may soil underwear.
-
Blood on toilet paper.
-
Difficulty controlling bowel movements
Anal fistula symptoms may come and go, with periods of improvement and flare-ups. Symptoms can also worsen during periods of infection or if new perianal abscesses form.
Many people with anal fistulas have a history of a perianal abscess weeks or months earlier, which may have drained or been surgically treated.
Although anal fistula symptoms can cause embarrassment and anxiety, it’s important to understand that they aren’t caused by poor hygiene and that they can be treated effectively with surgery.
If you think you have an anal fistula and are experiencing any of these symptoms, you should seek medical evaluation. Early diagnosis and treatment can prevent complications and improve treatment outcomes.
What causes anal fistulas?
Most anal fistulas are caused by a perianal abscess, where an abscess filled with pus develops around an infected anal gland, creating a pocket that forms into a tunnel when the abscess drains.
Anal fistulas can have other causes, including:
-
Crohn's disease – an inflammatory bowel disease
-
Previous anal surgery or trauma
-
Radiation therapy (for pelvic cancers)
-
Diverticulitis – inflammation of pouches (diverticula) in the digestive tract
-
Hidradenitis suppurativa – a chronic skin condition
-
HIV/AIDS
-
Tuberculosis (rare in the UK)
-
Sexually transmitted infections (rare)
-
Cancer (a very rare cause)
Risk factors that can make it more likely you’ll develop anal fistulas include:
-
A history of perianal abscess
-
Having an inflammatory bowel disease, such as Crohn's disease or ulcerative colitis
-
Having diabetes
-
Having a weakened immune system
-
Anal trauma
-
Chronic diarrhoea
In most cases, there’s no underlying condition beyond the abscess itself – the fistula simply develops as a complication of anal gland infection. Anal fistulas are not caused by poor hygiene, and they are not contagious.
Understanding the cause of your anal fistula is important for treatment planning and preventing recurrence.
Diagnosing an anal fistula
Diagnosing an anal fistula typically involves:
-
Physical examination – Your consultant will examine the area around the anus to look for signs of an external opening, as well as swelling, redness, or any indications of pus drainage.
-
Digital rectal examination (DRE) – Your consultant may gently insert a gloved finger into the anus to feel for any abnormalities, like internal openings, and to assess the sphincter muscles.
-
Goodsall's Rule - This is a surgical guideline used for predicting the path of an anal fistula based on the location of the external opening.
Diagnostic investigations
In addition to clinical examination, the following may be used to aid the diagnosis:
-
MRI scan – This is the gold standard for assessing fistula anatomy, as it clearly shows the fistula path, any branches, and its relationship to the sphincter muscles.
-
Endoanal ultrasound – An alternative or complementary imaging technique to MRI for visualising the fistula tract.
-
Examination under anaesthesia (EUA) - This can be performed by a surgeon to thoroughly explore the fistula tract and surrounding anatomy, usually when dealing with complex cases or before surgery to accurately assess the fistula.
-
Fistulography - A specialised X-ray procedure that uses a contrast dye to visualise the fistula tract. This is less commonly used now.
-
Colonoscopy - A procedure where a long, flexible tube with a camera (a colonoscope) is inserted into the anus to visually examine the anal tract from the inside. This may be performed if Crohn's disease is suspected.
Your surgeon will use a classification system to categorise your fistula type, which guides treatment decisions. Accurate assessment is crucial as it determines the best surgical approach to take.
Your consultant will discuss the diagnostic findings with you and explain the treatment options available for your specific case.
Anal fistula treatment options
Anal fistulas very rarely heal on their own without intervention. Surgery is usually the most definitive treatment, with the highest rate of success and lowest risk of recurrence.
A range of procedures can be used to treat anal fistulas. Which procedure is right for you will depend on the type and complexity of your fistula, the amount of sphincter muscle involved, your continence status, your surgeon’s expertise, and the presence of other conditions, like Crohn's disease.
Conservative management
Conservative (non-surgical and light surgical) treatments are rarely curative on their own, but may be used as part of a staged treatment approach or to manage specific situations:
-
Seton placement – A surgical thread placed through the fistula tract. This can be used as a temporary measure before definitive surgery or as part of a staged procedure. It drains infection and allows healing around the tract. In complex fistulas or for patients with Crohn's disease, a seton may be left in place long-term.
-
Medical management for Crohn’s-related fistulas – Biologic medications and immunosuppressants may help heal some fistulas in patients with Crohn's disease, but surgery is often still needed for complete treatment.
Surgical treatment overview
There are different types of anal fistula surgery, but the goal of each procedure is to cure the fistula and to preserve continence (the ability to control your bowels).
Most anal fistula operations are performed as outpatient procedures, meaning you’ll go home the same day as your operation. In some cases, patients may stay overnight. This is usually when the surgery is complex, there are difficulties managing pain, or if there are any other medical complications.
Anal fistula surgeries are done with you under anaesthesia, usually either general anaesthesia (putting you to sleep) or spinal anaesthesia (numbing the area).
There are multiple surgical options available, and your surgeon will recommend the best anal fistula surgery for you based on your individual case.
Types of anal fistula surgery
Fistulotomy
With a fistulotomy, the surgeon cuts the anal fistula tract open (laying it bare) to allow healing from the tract upwards.
Fistulotomies are the most common type of anal fistula surgery performed and are most likely to be done so for simple fistulas involving minimal crossing of the sphincter muscle (typically intersphincteric or low transsphincteric anal fistulas).
The procedure
The details of fistulotomies can vary, but typically they involve:
-
General or spinal anaesthesia
-
Using a probe to identify the fistula tract
-
Cutting open the fistula tract along its entire length
-
The wound being left open to heal naturally from the inside out
-
The wound may be packed initially
The operation typically takes between 20 to 45 minutes, depending on the complexity of the fistula tract.
The advantages of a fistulotomy
-
It’s considered the gold standard operation for simple fistulas with the highest rate of success
-
It’s a straightforward technique, and one procedure is usually sufficient to cure the fistula
-
Fistulotomies have the lowest recurrence rate
Fistulotomy considerations
-
There is a small risk of minor and temporary continence changes after the procedure, such as minor leakage and increased urgency
-
The surgical wound can take some time to heal, typically between 6 to 12 weeks, and will require wound management to heal properly
-
Post-operative wound care is crucial for proper healing
-
A fistulotomy usually isn’t suitable for complex or high fistulas where too much of the sphincter would be divided
LIFT procedure (Ligation of Intersphincteric Fistula Tract)
The LIFT procedure is a newer sphincter-preserving technique designed to treat transsphincteric fistulas. During the operation, the surgeon identifies the fistula tract in the space between the internal and external sphincter muscles and securely ties it off.
This approach aims to eradicate the fistula while avoiding damage to the sphincter muscles, thereby significantly reducing the risk of continence problems. The procedure is often performed as a day-case operation, meaning you can go home the same day as the operation.
Advanced flap repair
This approach involves covering the internal opening of the fistula with a flap of healthy tissue taken from the rectal or anal canal lining.
It’s most commonly used for high or complex fistulas, particularly in women (where the sphincter is shorter) or those with Crohn’s disease. This technique avoids dividing the sphincter muscles, and in some cases, further procedures may be required if the fistula does not heal fully after the first operation.
A fistula plug or glue
Fistula plugs and fibrin glue are minimally invasive treatment options in which the fistula tract is filled rather than surgically opened.
A bioabsorbable plug or medical adhesive is used to seal the tract from within, allowing the body to heal around it. These techniques carry very little risk to sphincter function and usually involve a quicker recovery. However, the materials used can be costly, increasing the cost of the procedure. Fistula plug or fibrin glue are often tried as a first option before more invasive surgery in complex or high fistulas.
VAAFT (Video-Assisted Anal Fistula Treatment)
VAAFT is a minimally invasive endoscopic technique that allows the surgeon to see inside the fistula tract using a small, slender camera (an endoscope) to guide the operation, which is performed using “keyhole surgery” tools.
The fistula tract is cleaned and destroyed from the inside, and both the internal and external openings are then closed. This method aims to precisely treat the fistula while minimising tissue damage. Although early results are promising, VAAFT is a relatively new technique, and data on long-term outcomes are still limited.
Staged anal fistula procedures
Staged procedures are used for more complex fistulas where a single operation may carry a high risk of incontinence.
A cutting seton may be placed and gradually tightened over weeks or months, allowing the fistula to be divided slowly while scar tissue forms to maintain sphincter control. Alternatively, a two-stage fistulotomy may be performed, with an initial seton placed to control infection, followed by definitive surgery at a later date.
These staged approaches are specifically designed to balance effective fistula treatment with protection of continence function and can be tailored to specific and complex cases.
Choosing the right anal fistula procedure
The decision on what is the best kind of fistula surgery for you will depend on a range of factors. This includes:
-
The complexity and height of the fistula
-
The degree of sphincter involvement
-
Your risk of incontinence
-
Whether you’ve had any previous fistula surgeries
-
Any other underlying conditions you might have, such as inflammatory bowel disease
In some cases, more than one procedure may be necessary to cure your fistula, especially in complex cases. Your Ramsay surgeon will review your case in detail and will discuss the risks and benefits of each option with you to ensure the best option is picked for you and that you understand what it involves.
Preparing for your anal fistula surgery
You’ll receive detailed instructions on how to prepare for your anal fistula surgery, but this will typically involve:
-
Fasting - Typically, you won’t eat for 6 hours before your procedure and won’t drink for 2 hours beforehand.
-
Bowel preparation - You may require an enema on the morning of the surgery to empty your rectum.
-
Medication - If you regularly take medication, you’ll be advised on which one you can continue to take and which you should stop before your surgery (such as blood thinners).
-
Arrange transport home - You won’t be able to drive yourself home after your operation due to the after-effects of the anaesthetic. And you likely won’t be able to drive for a week or two after the procedure.
-
Time off work - Plan time off work after your operation, usually 1 to 2 weeks for sedentary jobs and 4 to 6 weeks for more active work.
-
Stock supplies at home - Make sure you already have everything you need before your operation, including painkillers, high-fibre foods, stool softeners, sanitary pads, and plenty of comfortable, loose clothing.
What to expect on the day of your anal fistula surgery
Most anal fistula surgeries are performed as day-case procedures, meaning you'll go home the same day. On the day of your surgery, you can expect:
-
Admission around 2 to 3 hours before your surgery
-
Completing the consent process and final checks
-
Meeting your anaesthetist and surgical team.
-
Surgery, taking between 30 to 60 minutes, depending on the complexity of your case.
-
Resting in a recovery area for around 1 to 2 hours.
-
Going home the same day once you’ve recovered (some patients may stay overnight if advised to do so)
Recovery after anal fistula surgery
Your recovery will depend on a range of factors, including what kind of surgery you had, how complex your fistula was, your general condition, and how well your body heals.
Here’s a general guide to what you can expect following anal fistula surgery:
The first 24–48 hours of your anal fistula surgery recovery
During the first one to two days after your surgery:
-
Moderate pain is expected - usually less severe than abscess pain and manageable with medication
-
Take prescribed painkillers regularly
-
Wound packing – may be present and will be removed at first dressing change (usually day 1-3)
-
Discharge (blood or clear fluid) from the wound is normal
-
Use sanitary pads to protect clothing and stay comfortable
-
Eat and drink normally – focusing on high-fibre foods and hydration
-
Rest but move gently to aid healing
-
Difficulty passing urine may occur initially – contact the hospital if you cannot pass urine within 12 hours.
The first week of your anal fistula surgery recovery
-
Pain typically worsens during the first 3-4 days, then gradually improves
-
Stronger pain relief may be prescribed depending on your situation
-
Your first bowel movement usually occurs within 1-3 days after surgery
-
Take stool softeners from day 1
-
Eat high-fibre foods and drink plenty of fluids
-
Follow wound care advice
-
Sitz baths after bowel movements – sit in warm water for 10-15 minutes
-
Avoid prolonged sitting
-
No heavy lifting or strenuous activity
-
Gentle walking is encouraged
-
Continue high-fibre diet and plenty of fluids
Weeks 2 to 4 of recovery
-
Pain continues to improve
-
Wound heals from base upwards – may look deep initially, which is normal
-
Discharge gradually reducing
-
Bowel movements become more comfortable
-
Follow your established wound care routine
-
Gradually increase activity levels
-
Many patients return to light work during weeks 2-3
-
Avoid heavy lifting – nothing over 5kg
-
More normal daily activities are possible
-
Follow-up appointment usually scheduled during this period for wound assessment
Weeks 5 to 8 of your anal fistula surgery recovery
-
Wound significantly smaller as it heals from the inside out
-
Less discharge and discomfort
-
Return to normal activities, including work and gentle exercise
-
Continue high-fibre diet
-
Occasional sitz baths may still be helpful
-
Healing continues beneath the surface
Your long-term healing
Complete healing typically takes 6-12 weeks, depending on wound size and surgery type.
A small percentage of patients may experience minor continence changes initially, such as urgency, difficulty distinguishing gas from stool, but these symptoms usually improve with time.
Follow-up appointments with Ramsay help monitor your progress and address any concerns
Risks and complications of anal fistula surgery
Although anal fistula surgery is generally safe, complications can occur. The level of risk varies depending on the type of procedure and the complexity of your fistula.
When to seek urgent medical advice
You should seek urgent medical advice if you:
-
Cannot pass urine at all within 12 hours of your operation
-
Have heavy bleeding
-
Experience severe pain that can’t be controlled by medication
-
Have a fever above 38°C
-
Experience increasing redness, swelling, or pus from the wound
-
Have a sudden loss of bowel control
Living with a healing anal fistula wound
After your surgery, you’ll have to look after your healing surgical wound, typically for between 4 to 8 weeks.
Living with a healing anal fistula wound requires patience and a consistent daily routine. Proper wound care is the cornerstone of successful healing and helps reduce discomfort, infection risk, and delays in recovery. While the process can feel slow at times, most people notice steady improvements day by day.
We’ll give you detailed instructions on how to take care of your healing surgical wound, including in writing. Typically, you should expect the following:
Daily wound care
-
Shower once a day – a gentle stream of warm water over the wound is usually sufficient
-
After bowel movements – soak in a warm sitz bath for 10-15 minutes to ease discomfort and cleanse the area
-
Pat dry carefully – don't rub the wound
-
No creams or ointments unless specifically prescribed
-
Wear loose cotton underwear
-
Change sanitary pads regularly to manage drainage
Dietary management
-
High-fibre diet – with fruits, vegetables, whole grains, and legumes
-
Drink plenty of water to stay hydrated
-
Avoid foods that may harden your stools initially, such as white bread.
-
Fibre supplements may be needed for a short period
-
Maintain regular meal times to help establish predictable bowel habits
Activity modifications
-
Avoid prolonged sitting – take regular standing breaks
-
Use a cushion when sitting if needed
-
Gentle walking is encouraged to support circulation and healing
-
Avoid strenuous exercise and heavy lifting for 4-6 weeks
-
Swimming is typically safe once the wound has healed (usually after 2-3 weeks, but check with your surgeon first)
-
Gradually increase activity over time as you heal
Work considerations
-
Desk-based jobs – may return after 1-2 weeks
-
Physically demanding roles – may require 2-4 weeks or longer, depending on demands
-
Driving can usually resume once sitting is comfortable and pain is well controlled (typically after 1-2 weeks)
Managing discharge
-
Discharge is normal and can continue for several weeks after the procedure
-
Use sanitary pads – may need them for several weeks
-
Change pads frequently to protect clothing and skin
-
Moisture barrier cream may be recommended for the skin around the wound (not inside it) if irritation occurs
Sexual activity
-
Wait until comfortable – usually at least 3-4 weeks minimum
-
Some may need longer, particularly after more extensive surgery
-
Discuss with your surgeon if you have any concerns
Emotional support
-
Recovery can be frustrating – it's common to feel embarrassed or anxious
-
Anxiety around bowel movements is normal initially
-
Symptoms improve steadily as healing progresses
-
Support is available – reassurance, clear information from healthcare professionals, and support groups can make recovery easier to manage
Anal fistula surgery cost
The cost of anal fistula surgery varies depending on the type of surgery you require and where you choose to have your operation.
At Ramsay, we’ll give you a personalised quote for your anal fistula surgery after a consultation with one of our surgeons, which will then be valid for up to 60 days.
We offer a range of ways to pay, including:
-
0% Payment Plans – Allowing you to spread the cost of your anal fistula surgery across our flexible payment plans with fixed, monthly payments over a time period that suits you.
-
Self-fund treatment – All-inclusive Total Care – a one-off payment at a pre-agreed price that covers all the treatment you need.
-
Use your insurance – Your private healthcare insurance may cover your anal fistula surgery. We recommend that you obtain written confirmation from your insurance provider before starting your treatment with us.
Why choose a private anal fistula surgery
Choosing private healthcare for your anal fistula surgery means you can access treatment when you need it, as well as many other benefits, including:
- Enhanced privacy and dignity – Your own private room throughout your stay, giving you the comfort and discretion you need during recovery from this sensitive condition.
- Faster access to treatment – Private care means you can schedule your surgery quickly, at a time that suits you rather than being placed on a lengthy waiting list.
- Continuity of care – You'll be looked after by the same consultant from initial consultation through to discharge, building a relationship with a specialist who understands your individual treatment plan.
- Flexible appointments – Appointments arranged at times that work around your busy lifestyle from your initial appointment through to post-operative care.
Anal fistula surgery at Ramsay Health Care
At Ramsay Health Care, we specialise in colorectal procedures, including anal fistula surgery, combining expert surgical care with the personalised support you need throughout your recovery.
Your Ramsay experience:
-
Convenient locations across the UK, with most hospitals offering free on-site parking.
-
State-of-the-art facilities equipped with the latest surgical technology.
-
Personalised treatment plans tailored to your specific fistula type and complexity.
-
Patient-focused care from consultation through to discharge.
Ready to take the next step? Contact us today to speak to one of our advisors about anal fistula surgery at Ramsay Health Care and to book your consultation, you can also research specialists and book online for your consultation if that suits you.


