Osteoarthritis of the knee is a progressive joint condition where your cartilage gradually wears away, leading to pain, stiffness, and reduced mobility. It is the most common form of arthritis affecting the knee, typically worsening over time. Various treatments including osteoarthritis knee exercises, medication, injections, and, in severe cases, surgery, can help manage symptoms and improve your quality of life.
By understanding OA and exploring the available osteoarthritis knee treatment options can help you to take an active role in protecting your knee health and maintaining mobility.
What is knee osteoarthritis?
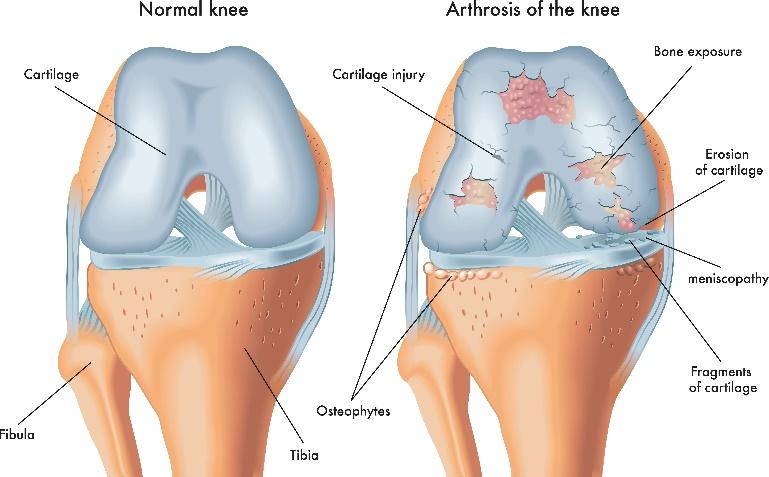
Knee osteoarthritis is a common condition that develops when the cartilage in your knee joint wears down, causing your bones to rub together. This leads to pain, swelling, and stiffness, and makes movement more difficult.
As a degenerative joint disease, OA is a result of wear and tear over time and can gradually worsen. Factors like age, previous injuries, genetics, and excess weight can increase your risk.
While there is no cure for osteoarthritis in the knee, treatments such as lifestyle adjustments, osteoarthritis knee exercises, pain management, and, in severe cases, surgery can help slow its progression and improve mobility. If knee pain is affecting your daily activities, you should seek medical advice to help determine the best approach to manage your symptoms.
Symptoms of knee osteoarthritis
Osteoarthritis knee symptoms may include:
- Pain – is often worse after activity, but it can also occur at rest or during the night in more severe cases.
- Stiffness - especially in the morning or after sitting; this usually improves within 30 minutes.
- Swelling - may be caused by fluid build-up or bony growths.
Grinding or cracking sounds - known as crepitus, happens when moving your joint. - Instability - your knee may feel like it could give way or lock occasionally.
- Reduced movement - difficulty bending, straightening, or walking.
You might also notice changes in your mood or sleep due to persistent discomfort. If symptoms are affecting your daily life, speak to your healthcare provider for support and treatment options.
Stages of knee osteoarthritis
While there aren’t strict medical stages defined for knee osteoarthritis, it is a progressive, degenerative condition that tends to follow a predictable path. Your healthcare provider might use stages to describe how advanced your knee OA is and to guide your treatment options.
Understanding the stages of osteoarthritis in knees can help you to track your symptoms and discuss long-term management options with your healthcare provider.
Here’s a general breakdown of the stages:
Stage 1 Osteoarthritis (Minor)
You may have early signs of cartilage wear in your knee, but typically no noticeable pain or discomfort. This stage might be detected incidentally through imaging, even if symptoms aren’t present.
Stage 2 Osteoarthritis (Mild)
This is often when people first start to notice symptoms, such as occasional pain or stiffness, especially after physical activity. There’s still enough cartilage to cushion the joint, but some damage is beginning.
Stage 3 Osteoarthritis (Moderate)
By this stage, the cartilage is noticeably worn, leading to increased pain, especially with walking, bending, squatting, or climbing stairs. You may also experience swelling, stiffness, or limited movement, particularly after rest.
Stage 4 Osteoarthritis (Severe / End Stage)
At the severe stage, most or all of your cartilage has worn away, and your bones may rub against each other. This can cause intense, persistent pain, significant stiffness, and limited mobility. For some people, this stage may lead to considering joint replacement surgery.
Complications of knee osteoarthritis
While knee osteoarthritis often progresses slowly, it can lead to a range of complications over time. These include:
- Joint instability - as cartilage wears away and muscles weaken, your knee can become unstable and feel like it might “give way” and this can also increase your risk of injury.
- Bone spurs (osteophytes) - bony growths can form at the edges of your joint where cartilage has been lost. They can cause further pain, stiffness, and reduced joint movement.
- Baker’s cyst - a fluid-filled swelling at the back of your knee can occur if joint fluid bulges through a small tear in your joint capsule. It may not always be painful, but if it bursts, it can cause sudden pain, swelling, and redness in your calf.
- Altered gait and posture - pain and stiffness in your knee can change how you walk and move. Over time, this altered movement can place strain on other joints, such as your hips or lower back, potentially leading to additional joint problems.
- Reduced mobility - ongoing pain and stiffness may limit your ability to carry out daily activities, impacting independence and quality of life.
- Mood changes - due to chronic pain, reduced mobility and interference with daily life and sleep can lead to emotional challenges.
If you're concerned about any of these complications, speak with your healthcare provider. Early management and support can help reduce their impact and maintain your quality of life.
Causes of knee osteoarthritis
An osteoarthritis knee occurs when the cartilage in your knee joint gradually wears down, leading to pain, stiffness, and reduced mobility.
Cartilage acts as a protective cushion, covering the ends of your bones and allowing smooth, friction-free movement. It also absorbs impact, reducing strain on your joint when walking or standing. However, once cartilage starts breaking down, it cannot regenerate, making movement increasingly difficult over time.
Maintaining joint health through exercise, weight management, and proper movement can help slow OA progression and reduce discomfort.
Risk factors which may contribute to knee osteoarthritis
You may be more likely to develop osteoarthritis in your knees if:
- You have a body mass index (BMI) of 30 or more (classified as overweight or obese)
- You’ve had a previous knee injury or ongoing joint problems
- Your job or sport involves repetitive stress or heavy use of the knees
- You have a family history of osteoarthritis
- Your bones or joints are misaligned, such as having knock knees or bowlegs
- You're over the age of 50, as risk increases with age
- You have other joint conditions, like rheumatoid arthritis or gout
- You're female - women are more likely than men to develop knee OA, especially after menopause.
Understanding your risk factors can help you take steps to protect your joints early on.
How to prevent osteoarthritis in the knees
While osteoarthritis of the knee cannot always be prevented, reducing strain on your joints can lower your risk and help maintain knee health. Small adjustments in daily activities, fitness routines, and lifestyle choices can make a big difference. These include:
- Modify activities that put stress on your knees - if your job requires frequent kneeling or heavy lifting, consider adjustments to reduce impact.
- Opt for softer surfaces when exercising - running on grass or tracks instead of pavement can lessen strain on your joints.
- Include low-impact exercises - swimming, cycling, or strength training help maintain fitness without excessive knee stress.
- Maintain a healthy weight - losing even 10% of excess weight can significantly ease knee pressure and lower OA risk.1
How is osteoarthritis of the knee diagnosed?
If you're experiencing knee pain, stiffness, or mobility issues, your specialist will begin with a comprehensive assessment to determine if osteoarthritis is the cause. This includes:
- Physical examination - checking for swelling, tenderness, discoloration, or signs of previous injury.
- Pain assessment - identifying whether discomfort is localised or widespread in your joint.
- Range of motion - evaluating how freely and comfortably your knee moves.
- Joint stability - assessing whether your knee feels loose or unstable during movement.
- Gait analysis - observing how you walk and bear weight on the affected knee.
To confirm your diagnosis, imaging tests may be required:
- X-ray - a key tool for detecting cartilage loss, joint space narrowing, or bone changes associated with osteoarthritis.
- MRI or CT scan - occasionally used to provide detailed images of soft tissues, particularly if further examination of ligaments or cartilage is needed.
Knee osteoarthritis treatment
Knee osteoarthritis is a progressive condition where cartilage wears down over time, leading to pain, stiffness, and reduced mobility. While there isn’t a cure for osteoarthritis in knee, treatment focuses on reducing pain, improving movement, and maintaining knee function.
Osteoarthritis knee treatment options range from lifestyle changes and medications to injections and surgery, depending on severity and your individual needs.
Specialists at Ramsay Health Care can assess and help treat your knee osteoarthritis with medications including injections, physiotherapy and surgery.
Medication
Medications to treat knee osteoarthritis may include:
- Topical pain relief - NSAID or capsaicin creams or gels applied directly to your knee.
- NSAID tablets - oral anti-inflammatory medications, often prescribed with stomach-protecting medication to reduce side effects.
- Paracetamol - common pain reliever for mild to moderate discomfort.
- Opioids - stronger painkillers, prescribed for short-term use.
- Steroid injections - corticosteroid injections directly into your knee joint to reduce inflammation and pain.
- Supplements - some people take glucosamine or chondroitin, though evidence of their effectiveness is limited.
Physiotherapy
Physiotherapy plays a key role in managing knee osteoarthritis by helping strengthen muscles, improve mobility, and reduce pain. A physiotherapist will design a personalised rehabilitation program with targeted osteoarthritis knee exercises to support joint function and stability. Physiotherapy options include:
- Exercise therapy - strengthening leg and knee muscles can improve support and help maintain movement.
- TENS therapy - some patients benefit from transcutaneous electrical nerve stimulation (TENS), which uses mild electrical currents to reduce pain signals.
- Braces and supports - physiotherapists may recommend knee braces to provide stability and support alongside other treatments.
- Occupational therapy - an occupational therapist can suggest modifications at home and work, such as bath aids, grab rails, or stair supports, to make daily activities easier.
Exercise for knee osteoarthritis
Staying active is essential for managing knee osteoarthritis. Regular movement helps reduce stiffness, strengthen muscles, and improve mobility, allowing your knee to better cope with daily activities.
Finding the right balance is key - too much activity can worsen pain, while too little may cause stiffness. A mix of gentle movement and rest helps maintain mobility and reduce discomfort. Keeping up with osteoarthritis knee exercises is also crucial, even as symptoms improve, to maintain strength and prevent regression.
A physiotherapist can help tailor an exercise plan to your needs, ensuring safe and effective movement strategies. Here are some exercises that help treat knee osteoarthritis:
- Range of motion exercises - simple stretching and mobility exercises help maintain flexibility and improve posture.
- Strengthening exercises - focused workouts help stabilise the knee, reduce pain, and prevent falls. Aim for at least two sessions per week.
- Aerobic exercise - activities like cycling, walking, and swimming can boost fitness while reducing pain through endorphins. Try to get 2.5 hours per week spread out over several days.
- Hydrotherapy - exercising in warm water can be soothing and supportive, particularly if movement on land is difficult.
Injections
Injections to treat knee osteoarthritis include:
- Cortisone (steroid) injections - help reduce inflammation and pain by delivering corticosteroids directly into the knee joint.
- Knee gel shots (viscosupplementation) - contain hyaluronic acid, which helps lubricate your joint, easing pain and improving mobility.
- Genicular nerve block injections - target the nerves around your knee, blocking pain signals for temporary relief in more advanced cases.
- Platelet-rich plasma (PRP) injections - use platelets from your own blood to promote healing and reduce inflammation in damaged knee tissues.
Surgery
If osteoarthritis causes severe pain or significantly affects daily life, surgery may be considered if other non-surgical treatments, such as exercise, weight management and medication are not successful. Common surgical options include:
-
Knee arthroscopy - a keyhole procedure used to remove loose cartilage or damaged tissue. While not typically recommended for OA, it may help if your knee locks or catches.
-
Osteotomy - your bone is cut and realigned to shift weight away from your damaged joint area. This surgery is often considered for younger patients (under 60) to prolong their natural knee function.
-
Partial knee replacement - only the damaged part of your knee joint is replaced with an artificial component. This preserves as much of your natural knee as possible.
- Total knee replacement - your entire knee joint surface is replaced to provide long-term pain relief and improved mobility for advanced OA cases. Knee replacement is the most frequently performed OA surgery, with advancements in the technique showing they last for 25 years.2